
Reset Your Future Bilingual Self: How Micro-Skills in Any Language Transform Care in 2026
by ACOI
January 5, 2026
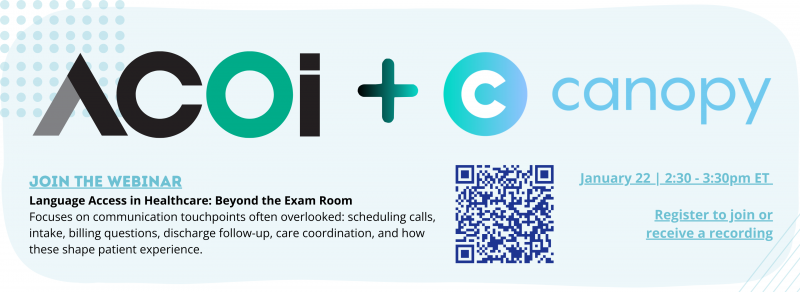
This post is part of our broader conversation on language access in healthcare. If this topic resonates, we invite you to register for our upcoming free webinar, Language Access in Healthcare: Beyond the Exam Room, on January 22 from 2:30 - 3:30 pm ET.
The session explores communication touchpoints that are often overlooked, including scheduling calls, intake, billing questions, discharge follow-up, and care coordination, and how these moments shape patient trust and experience just as much as what happens in the exam room. Registration is required, and all registrants will receive the recording, whether or not you can attend live.
The Moment Communication Changes Care
Every clinician and care-team member has a story about communication that changed everything.
Maybe it was the first time a patient’s shoulders dropped in relief because you greeted them in their preferred language. Maybe it was the family who finally understood a complex discharge plan after you slowed down and used teach-back. Or perhaps it was the day you realized how many of your patients with limited English proficiency (LEP) were nodding politely, but leaving the hospital confused and scared.
As we begin 2026, Canopy and ACOI are inviting you to imagine, and actively build, your future bilingual self: the version of you who can reliably build trust, dignity, and rapport with patients across languages and cultures, not by magic fluency, but through intentional habits and micro-skills. Members save 20% off Canopy, the #1 medical Spanish course in the US. Learn more.
Start with One High-Value Scenario
It’s easy to get overwhelmed by the idea of “becoming bilingual.” Instead, we encourage you to begin with one concrete scenario you care about: ED triage, primary-care intake, medication counseling, or discharge instructions.
Ask yourself: If I could wave a wand, what would excellent communication look like in this specific encounter for a patient with LEP or low health literacy? Use Canopy’s “Can Do” statements to write down a goal in your own words. For example, “I can elicit accurate symptom histories in [Spanish/etc.] using open-ended questions and clarifying prompts,” or “I can explain the top three red-flag symptoms and what to do if they happen.”
From there, identify 5-10 phrases plus one workflow habit (such as routine teach-back) that will move you closer to that goal. Revisit this scenario monthly to reflect on what’s getting easier and where you still feel stuck. That reflective cycle (goal, practice, reflection) is how your future bilingual self comes into focus.
Build Trust in the First 30 Seconds
Research and lived experience in emergency medicine and patient satisfaction are clear: the opening moments of an encounter have an outsized influence on how patients perceive their care. That’s even more true when language and cultural differences are in play.
You don’t need perfect grammar to make those first 30 seconds count. You do need a consistent opening that combines warmth, clarity, and transparency. In any language, that opener should include:
- A greeting and your name/role
- A quick check of language preference and need for interpretation
- Reassurance that you want them to understand and will bring in help as needed
A simple bilingual script like, “Hello, my name is… I’m your nurse/doctor today. What language do you prefer for your medical care?” followed by “My [Spanish/etc.] isn’t perfect, but I will use everything I know, and I will bring an interpreter so we can be very clear,” goes a long way toward reducing fear and signaling respect.
In busy EDs and clinics, these micro-openings are the difference between rushed, chaotic encounters and moments where patients feel safe enough to tell you what’s really going on.
Make Care Understandable, Not Just Delivered
Most of us were trained to be content experts, not communication experts. Yet our patients’ outcomes depend on what they actually understand, not on what we said.
One of the most effective habits you can build is the “chunk and check” pattern:
- Break information into small chunks: One problem, one action, one reason.
- Use patient-friendly language, not jargon.
- Ask the patient to restate what they heard in their own words.
- Gently correct and clarify as needed.
In practice, that might look like: “First, let’s talk about your inhaler. This medicine opens your airways so you can breathe more easily. Can you tell me when you’ll use it and how many puffs?” If the patient struggles, that’s not a failure; it’s a safety win. You’ve caught the confusion while you can still fix it, rather than after a preventable ED return.
In multilingual settings, this pattern works whether you’re using your own bilingual skills, an interpreter, or translated materials. Canopy’s curriculum is built to help you practice these structured explanations in Spanish and other languages, so they become muscle memory instead of one-off efforts.
From Personal Subscription to Institutional Change
Many Canopy users start by paying for their own license as students, residents, nurses, or allied staff. That personal investment is powerful, but it shouldn’t be the end of the story.
You’re already generating value for your institution: fewer miscommunications, smoother discharges, stronger rapport with LEP patients, and better compliance with language-access requirements. Those are exactly the outcomes your school, residency, hospital, or health plan is trying to achieve.
The next step is to translate your individual growth into a case for enterprise licensing, so your peers don’t have to keep paying out-of-pocket. Here’s a simple playbook:
- Collect 2-3 short stories or data points about how your bilingual skills or interpreter workflows improved a patient’s experience or safety.
- Identify a decision-maker: a residency or clerkship director, department chair, DEI or quality leader, or health-plan VP.
- Request a 20-minute conversation focused on how Canopy can support your program’s accreditation, equity, and workforce-development goals.
- Offer to be a “language-access champion” or pilot lead for your unit, residency class, or student organization.
- We do the rest.
By doing this, you’re not just building your future bilingual self; you’re creating the conditions for hundreds of future bilingual selves to grow alongside you.
A New Year, A New Story
January is full of resolutions that fade by February. This year, we’re inviting you to choose something different: one scenario, one opening script, one teach-back habit, and one advocacy step.
Those may look small on your calendar, but they add up to safer care, more trusting relationships, and a health system where language is no longer a barrier to dignity, understanding, or healing.
Your future bilingual self is already in motion every time you try a new phrase, call an interpreter early, or push your institution to do better. We’re here to make sure you don’t have to do that alone.
If you’re thinking about how language access shows up beyond face-to-face clinical encounters, we’d love to have you join us.
Register for our free January 22 webinar, Language Access in Healthcare: Beyond the Exam Room (2:30 - 3:30 pm ET) to dive deeper into real-world strategies for improving communication across scheduling, intake, billing, discharge follow-up, and care coordination.
Can’t attend live? Register anyway. All registrants will receive the full recording after the event.

