On October 31, the Centers for Medicare and Medicaid Services (CMS) released the CY2026 Medicare Physician Fee Schedule (MPFS) final rule that could have a significant effect on ACOI members depending on the mix of health care services they provide and where they provide them.
Among the finalized policies is a negative 2.5 percent “efficiency adjustment” that will be applied to the majority of physician services. CMS was unswayed by comments from ACOI and others opposing the sweeping efficiency adjustment and maintained the position that current valuations for the vast majority of services do not account for efficiencies gained in the delivery of services over time.
In the days ahead, ACOI will analyze the rules and report on specifics that may impact your practice and your patients.
2026 Conversion Factor
For 2026, conversion factors (CF) are based on whether a physician is an alternative payment model (APM) qualified participant (QP). The CF is the starting point for calculating physician payments under the MPFS. The CF is the dollar amount by which geographically adjusted RVUs are multiplied to arrive at the payment amount for a given service.
Non-APM QP $33.4009 (+3.26% change from 2025)
APM QP $33.5675 (+3.77% change from 2025)
The conversion factors reflect statutory adjustments, including the 2.5 percent positive adjustment provided by Congress earlier this year, a positive 0.49 percent budget-neutrality adjustment resulting from misvalued code changes, and the -2.5 percent efficiency adjustment.
Efficiency Adjustment
- A -2.5 percent efficiency adjustment will be applied to the work relative value units (RVUs) and corresponding intraservice portion of physician time for non-time-based services. The impact of the efficiency adjustment will depend on a physician’s mix of services with physicians who provide diagnostic services and tests, as well as procedures most severely affected. The efficiency adjustment does not apply to time-based services, including evaluation and management (E&M) visits, care management services, behavioral health services, and services on the CMS telehealth list. The only change CMS made to the final rule was exempting codes that are new for 2026.
- CMS uses the Medicare Economic Index (MEI) productivity adjustment percentage with a look-back period of five years to calculate the efficiency adjustment.
- CMS intends to apply the efficiency adjustment to the intraservice portion of physician time and work RVUs every three years with no floor of how much a service could be devalued.
Practice Expense
- CMS’ practice expense policy results in a dramatic shift of payment between sites of service. Facility-based payment to physicians will decrease overall by -7 percent while non-facility-based payment to physicians will increase by 4.
- The rule rejects the American Medical Association’s Physician Practice Information (PPI) Survey for updating 2026 practice expense (PE) relative values and instead reduces physician indirect PE payment when a physician provides services in a facility, even if they are not employed by the hospital. CMS states its new PE policy better reflects the rise in physicians in hospital-owned practices and physicians employed directly by a hospital and supports the Agency’s goals of site neutrality.
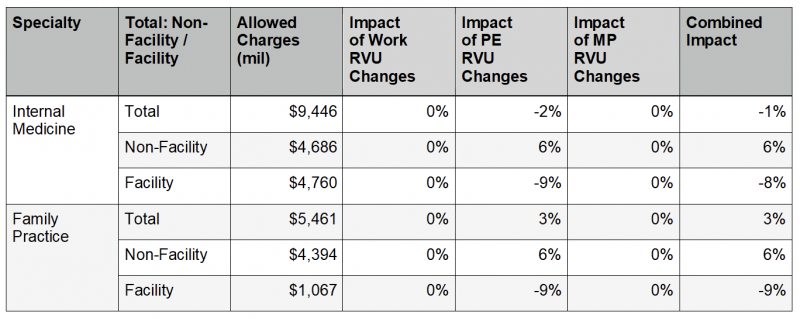
Source: Calendar Year 2026 Medicare Physician Fee Schedule Final Rule
Telehealth
- CMS has permanently lifted frequency limitations on telehealth services for subsequent inpatient visits, subsequent nursing facility visits, and critical care consultations.
- CMS has finalized, for services that are required to be performed under the direct supervision of a physician or other supervising practitioner, to permanently adopt a definition of direct supervision that allows the physician or supervising practitioner to provide such supervision through real-time audio and visual interactive telecommunications (excluding audio-only).
- CMS extended its current policy to allow teaching physicians to have a virtual presence in all teaching settings, in clinical instances when the service was furnished virtually, on a permanent basis. CMS had proposed to end this flexibility but reversed course in response to public comments.
Resources
CY 2026 Medicare Physician Fee Schedule Final Rule
CY 2026 Medicare Physician Fee Schedule Final Rule Fact Sheet


